Older adults with Alzheimer’s disease and related dementias (ADRD) face unique health challenges that can lead to higher reliance on Emergency Department (ED) care. While previous studies have evaluated other types of healthcare use such as hospitalization among patients living with ADRD, very little is known about ED visits. Understanding the reasons that bring patients with ADRD into the ED is an important first step to prevent potentially inappropriate visits.
This report demonstrates the use of national survey data to evaluate the characteristics of Emergency Department (ED) visits among patients living with Alzheimer’s disease and related dementias (ADRD).
The National Hospital Ambulatory Medical Care Survey (NHAMCS) is a nationally-representative, publicly available data source spanning from 1973–2022. NHAMCS collects patient visit data from a random sample of U.S. EDs located in all 50 states. Data are collected by trained reviewers who record information on patient characteristics, diagnoses, and visit characteristics such as services and treatment provided, as well as medications received. Unlike other commonly used data sources to evaluate ADRD care, NHAMCS also uniquely includes the primary reason for visit as reported by the patient and/or their proxy. Lastly, NHAMCS collects data across all payor types (i.e., is not limit to analysis of Medicare data). Here we demonstrate use of NHAMCS to examine the characteristics of ED visits among patients living with ADRD.
AUTHORS
Lauren Gerlach, DO, MS
University of Michigan
Jonathan Martindale, MHI
University of Michigan
Julie Bynum, MD, MPH
University of Michigan
Matt Davis, MPH, PhD
University of Michigan
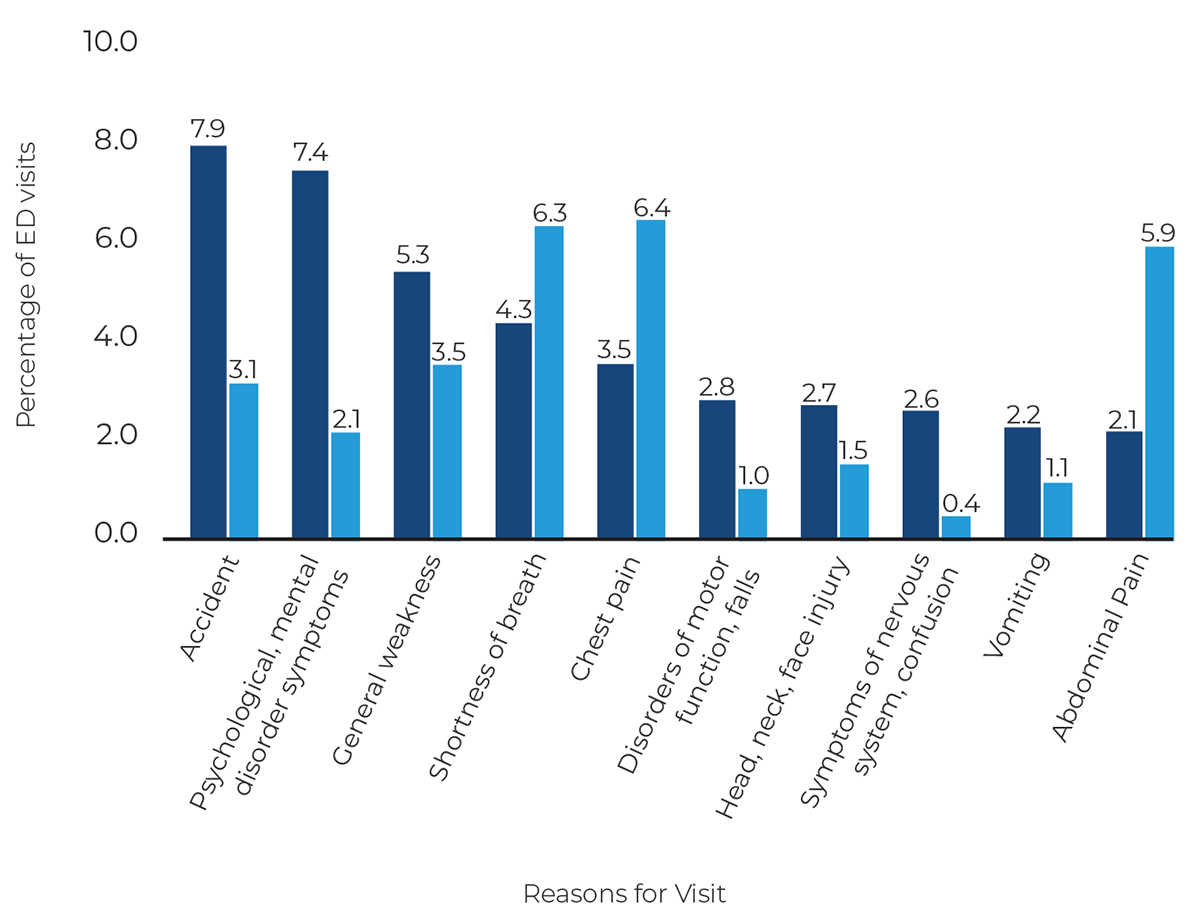
Figure 1
Top 10 primary reasons for visit among those with ADRD
| Patients with ADRD |
| Patients without ADRD |
What we did.
In this cross-sectional study we used data from the 2016–2019 NHAMCS to determine the most common reasons for visit and diagnoses associated with ED visits by ADRD status. All analyses were restricted to adults who were 65 years or older at the time of the survey and estimates were extrapolated to represent the U.S. older adult population. While there can be up to five reasons for visits coded, we selected the first reason for visit code which is the medical chief complaint or “most important” reason for visit reported by the patient and/or proxy reflecting their motivation for seeking medical care. Additionally, NHAMCS includes up to five diagnoses related to the visit which are based on the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes. This analysis focuses on the first listed and designated primary diagnosis related to the visit.
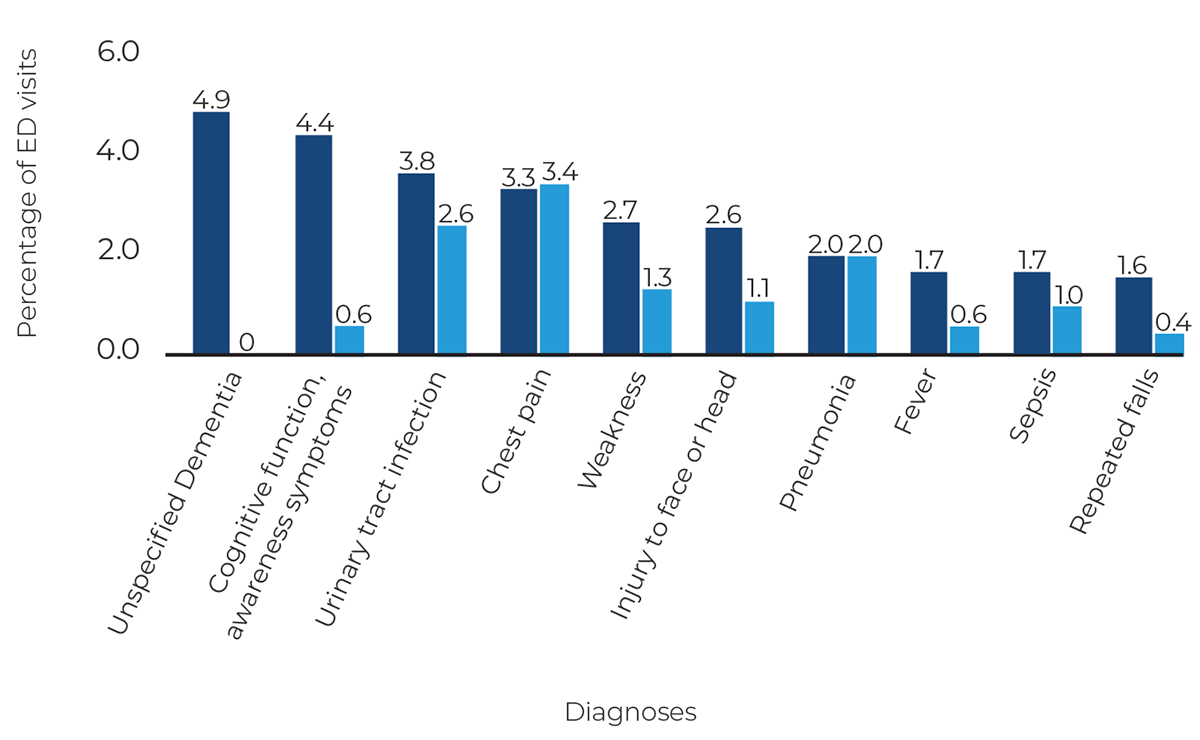
Figure 2
Top 10 primary diagnoses among those with ADRD
| Patients with ADRD |
| Patients without ADRD |
What we found.
Among more than 20.3 million annual ED visits by U.S. older adults, 1.4 million were by patients living with ADRD. This accounts for 7% of all annual ED visits by individuals age 65 and older. ED visits by patients living with ADRD were more common among those 85 years or older, female, and with greater medical comorbidity. The most common reason for visit among patients living with ADRD included accidents (7.9%) and behavioral and mental health disturbances (7.4%), which were twice as likely compared to non-ADRD visits. The most common ED diagnoses among patients living with ADRD included unspecified dementia with or without behavioral disturbances, symptoms involving cognitive function and awareness, and urinary tract infection.
What does this mean for ADRD research?
The high number of ED visits made by patients with ADRD annually signals the need for improved outpatient and caregiver support services to help prevent such visits.
This report demonstrates the use of national survey data to evaluate the characteristics of ED visits among patients living with ADRD. A distinct advantage of NHAMCS data is the ability to generate national estimates across all payor types and inclusion of patient and/or proxy reported reason for visit. The high number of ED visits made by patients with ADRD annually signals the need for improved outpatient and caregiver support services to help prevent such visits. With over 6 million U.S. adults currently estimated to have ADRD, such support services will be needed to reduce the risk of injury and prevent distressing behaviors that patients with ADRD can experience to minimize avoidable ED care.
The data used to create this brief report are available and can be found at the CAPRA data and training resources page.
Paper cited: “Characteristics of Emergency Department Visits Among Older Adults With Dementia,” JAMA Neurology. DOI:10.1001/jamaneurol.2023.2244